Booster shots work, but may not be needed when vaccines remain highly effective for most people
On Wednesday, the New England Journal of Medicine published a study from Israel that confirmed that giving a booster shot of COVID-19 vaccine to patients 60 and older greatly lowered infection rates and severe illness. However, this immediately followed the publication in The Lancet of an analysis showing that COVID-19 vaccines remain effective, continue to lower rates of infection and illness to a large degree, and as a result:
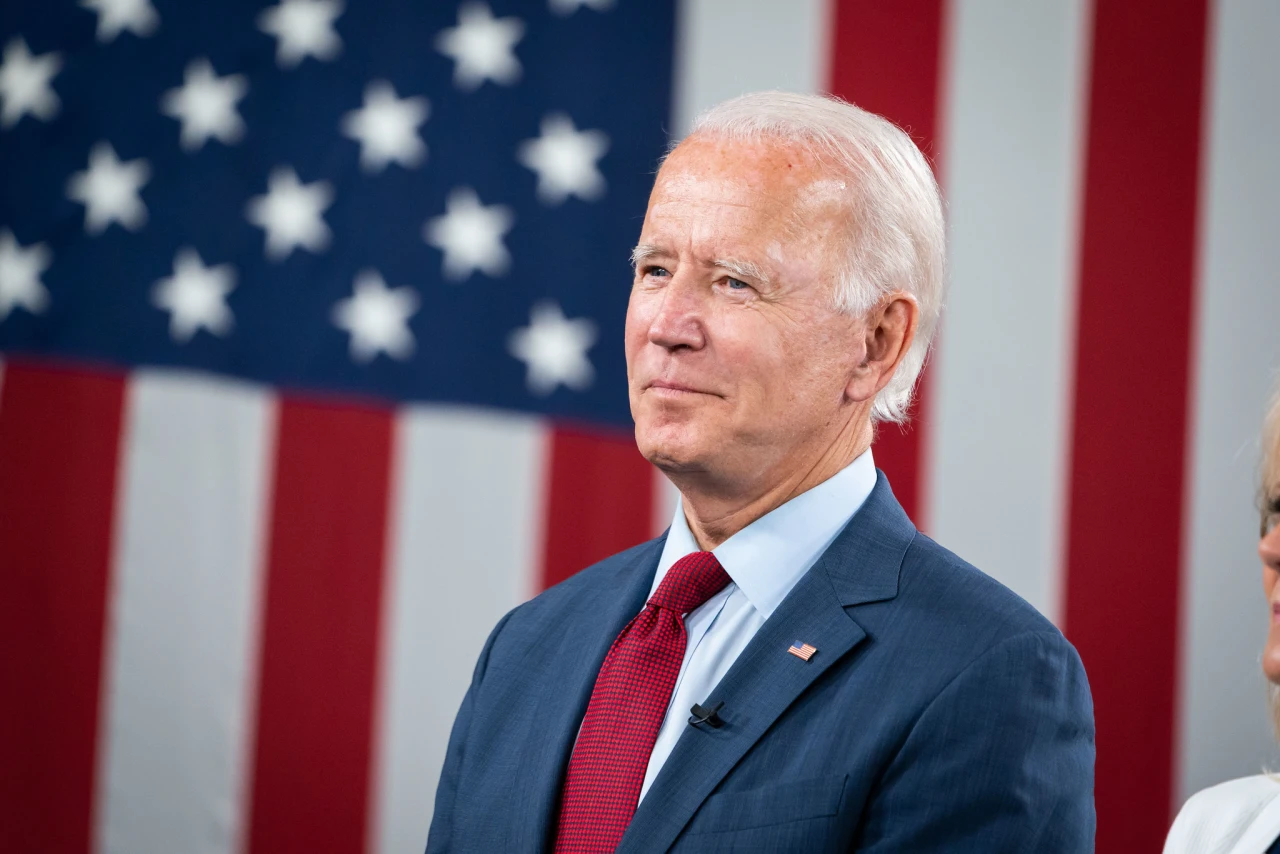
That conclusion might be getting less attention, except for the fact that the scientists behind it are the FDA team tasked with determining whether the U.S. needs to roll out a booster program. This seems to be in direct conflict with both statements that President Joe Biden made in his last address to the nation and recommendations coming out of the White House, which suggested a booster program that would begin on September 20.
Everyone agrees that boosters are vital for those whose immune systems are compromised. But the disagreement over whether they’re needed for the general population threatens to confuse most people about if, or when, a booster is necessary. And there’s another factor that the FDA analysis mentions, one that the World Health Organization has already voiced: Is it right for Americans to be taking a booster that might not be necessary when billions of people around the world are still lacking access to vaccines?
On the one hand, the conclusions from the FDA are very reassuring. That message is, despite the highly infectious delta variant, despite the high rate of hospitalizations in some areas, and despite a media focus on breakthrough cases, the current vaccines actually remain highly effective. Vaccinated individuals are still five times less likely to be infected. If they become infected, they’re eleven times less likely to develop serious illness. What’s happening in the United States now is not just a “pandemic of the unvaccinated” in the sense that those are the people filling hospital beds; it’s also the unvaccinated, to a large degree, who are spreading the disease.
None of this invalidates the Israeli study that indicated that receiving a booster greatly enhanced the immune response in patients over 60 and, at least over the duration of the study, reduced both their chances of infection and illness.
Those are substantial differences. Understandably, results like this are garnering a great deal of attention and increasing the clamor for boosters. However, there’s a point that’s easy to miss when looking at this analysis: By comparing the booster group only to those already vaccinated, the report obscures the fact that the vaccines already seem to be doing their job in a way that’s little short of miraculous.
The Israeli study looked at a population of 1,186,779 individuals over the age of 60, all of whom had been fully vaccinated at least five months earlier with two doses of the Pfizer vaccine. Of this group, 13,478 became infected in total. That’s 1.1% of the study population.
Beyond that, the study becomes more complex because some of the non-booster group people became members of the booster group. So, rather than deal with the results on a strict population basis, the study looked at “person-days” during which someone might have become infected or ill. Over 5.2 million person-days for the non-booster group, the study logged a total of 4439 infections. That’s about one infection for every three person-years of exposure. It also logged 294 cases of severe illness. Or about one severe illness per 48 person-years. Those are already excellent numbers. Bringing the odds of severe illness down to one in 591 years (the booster group result) is great … but is it really necessary?
And, of course it’s tempting to say “yes.” The vaccines may be “safe, effective, and save lives,” just as the FDA says, but there is definitely another factor to consider:
The best solution for the booster problem appears to be … don’t. Instead, send vaccines from the U.S. to the rest of the world and vaccinated people who have not had access to the vaccine so far. Give people around the planet the tremendous safety improvement that comes from being vaccinated in the first place, rather than adding more decimal places to the safety already enjoyed by vaccinated Americans.
Deploying the vaccines elsewhere rather than giving them to Americans might be the hardest political decision the FDA, CDC, and the White House could make. It’s almost certain to disappoint those who want that booster, as well as provide fodder to claims about the sinister nation of the WHO, or UN, or everything that’s outside the borders of “real America.”
But sending the vaccine to the unvaccinated isn’t just some grand humanitarian gesture. As the FDA points out, if a vaccine-resistant variant appears, that variant is almost certainly going to spring from the fertile ground provided by unvaccinated populations. The best thing that America can do to vaccinate ourselves as a nation is to see that everyone on the planet has access to vaccines. That’s more important right now than getting a third shot into the arms of the general population.
As a compromise, Biden could announce a program that provides booster shots to older Americans—say, those over 65. In the Israeli data, those over 70 were almost twice as likely to be infected as those between 60 and 70, and those over 80 had a much greater risk of severe illness. So picking an age and making boosters available to older Americans this month makes some degree of sense.
But don’t give a third jab to every American. Give the first shot to the rest of the planet. As the FDA researchers note: