Medicaid enrollments surged during pandemic, demonstrating how critical the program is
Ten million Americans gained health coverage through Medicaid and the Children’s Health Insurance Program from February 2020 through January 2021. That’s 10 million Americans able to gain and keep affordable health coverage, during a global pandemic, and in large part thanks to the Affordable Care Act and the Medicaid expansion it included. That was a 13.9% increase in enrollments in the program.
That’s coverage for a total of 80,543,351 people as of January, the Centers for Medicare and Medicaid Services reports. That included “over 38.3 million children … enrolled in Medicaid and CHIP combined, approximately 50% of the total Medicaid and CHIP enrollment.” That’s a big deal.
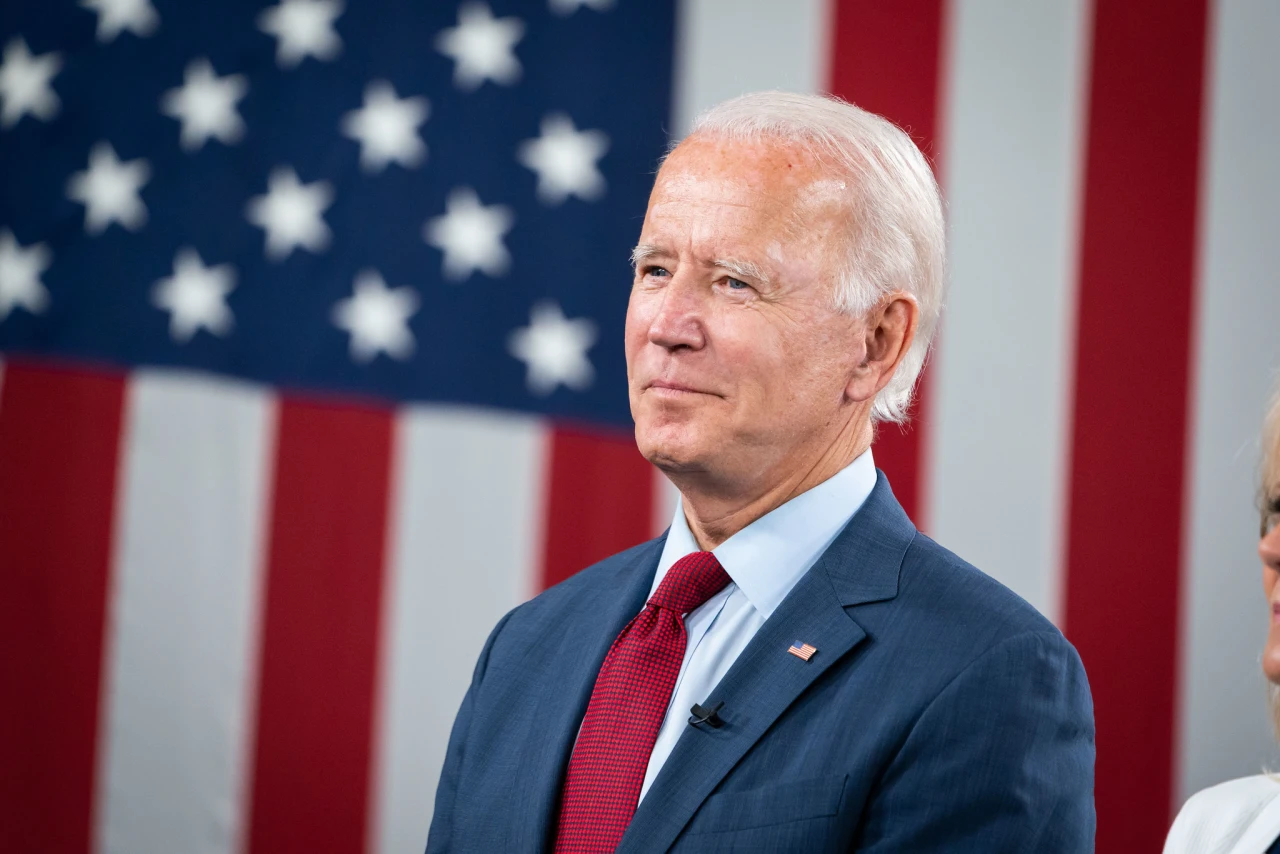
“The Biden-Harris administration is using every lever to ensure any American needing access to quality health coverage receives it. Now more than ever, people need the peace of mind of knowing that they have health coverage,” said Health and Human Services Secretary Xavier Becerra. “This report reminds us what a critical program and rock Medicaid continues to be in giving tens of millions of children and adults access to care. This pandemic taught us that now more than ever, we must work to strengthen Medicaid and make it available whenever and wherever it’s needed using the unprecedented investments Congress provided.”
One of the first COVID-19 relief bills the Congress passed, the Families First Coronavirus Response Act (FFCRA), provided states with a temporary 6.2% bump in federal matching for Medicaid. CMS says that the increase in enrollments can be “largely attributed” to that. President Biden reopened enrollment in the Affordable Care Act in April, lasting until Aug. 15. That’s likely to net more Medicaid enrollees who will find out they’re eligible for the program through the application process on Healthcare.gov in those states that expanded.
Biden’s COVID-19 stimulus package, the American Rescue Plan, included an estimated $22.5 billion in additional Medicaid funding for states that had not yet expanded the program. That was in part as incentive for those states to expand, but only one of the states—Wyoming—tried to do so. That effort failed when the state Senate killed the state House’s expansion bill. The state’s Medicaid enrollment is up 17% since COVID-19 hit anyway, according to Charles Gaba’s analysis. Between 15,000 and 25,000 uninsured people in Wyoming could get coverage if the state expanded Medicaid. (Gaba has analyzed Medicaid enrollments for all the states at ACASignups.net, if you’re curious to see what’s happening in the states.)
One of the things this big jump in enrollments during the pandemic has proven is just how key the program is in economic downturns. Adult enrollment grew twice as fast as enrollments in CHIP during the pandemic, showing that Medicaid was there for all the people who lost their jobs last year. “In past economic downturns there has been substantial growth in Medicaid enrollment but it was concentrated among children,” Rachel Garfield, co-director of the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, told The New York Times. “This time, it’s interesting we’re seeing much of the enrollment happening among adults.”
She also pointed out that this economic and public health crisis resulted in far more Medicaid enrollments than previous downturns—fewer than 4 million people signed up for Medicaid in 2009 at the height of the Great Recession. That can probably be attributed to two factors: This was a public health crisis and getting coverage has been critical, and secondly because of Obamacare, which didn’t exist in 2009. Because with expansion, more people qualify for the program.
Pamela Herd, professor of public policy at Georgetown University, has another explanation. “Reduction in burden mattered. Pandemic rules meant states couldn’t kick beneficiaries off Medicaid,” she tweeted. “Roughly 25% of Medicaid beneficiaries lose coverage w/in a year, and half of those are then uninsured (it’s call churn). Many lose coverage because they make paperwork mistakes.” She points out that Tennessee kicked 128,000 children out of the program because of paperwork issues in their 50-page application to keep coverage—the redetermination for eligibility. They just kicked the kids off without contacting parents to attempt to fix the errors. The public health emergency, in effect throughout 2021, prevents states from doing this.
“Medicaid and CHIP serve as a much-needed lifeline for millions of people throughout this country. The increase we are seeing is exactly how Medicaid works: the program steps in to support people and their families when times are tough,” said CMS Administrator Chiquita Brooks-LaSure. It’s hard to argue otherwise after the experience of the last 18 months.